Back in the day (12+ years ago) medical claims were completed by hand or type writer. I remember putting the claim in upside down, and rolling it up so that I could add in the patients information, subscriber information and the CPT, Modifiers, ICD-9, and charge amount. It was so tedious. The doctor would treat between 8-14 patients a day and we would complete the forms and mail everything out on Friday.
About 30-45 days later (varied by insurance carrier) we would get an Explanation of Benefit back explaining if the claim was approved or denied. We used to keep a paper ledger of our patients to track any claims not paid (like I said this was 12 years ago and our doctor was old fashioned. We begged for a computer).
12 years ago it wasn't a priority to go electronic because not all insurance carriers were accepting claims electronically but now it's a NECESSITY and any doctor that is still processing paper claims is outdated and actually losing money. Let me show you what I mean:

Medical offices that are sending claims by paper have to wait until they are first received at the insurance carrier. So, if we billed claims every Friday and it took 2 days for the post office to deliver the claims + 1 day for the insurance carrier to scan the claims into their software we are now 3 days out. It takes the insurance carrier 15-25 days to process the claim and then another 3-5 days to process the check and mail everything back to the doctors office.
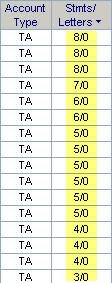
With good insurance carriers and if all things in the universe go right you will get your Explanation of Benefits with a check and a list of all patients that were denied along with those reason. Medical offices usually have collectors working on any past due or outstanding accounts that are 35+, 45+, 60+, 90+ and 120+ days old. Patients receive statements 35, 45, 65, 90 and sometimes over 180 days after treatment for co-payments, coinsurance and deductible balances. Mainly patients refuse to pay because they don't remember being treated, don't feel like they owe on such a old balance etc.
Doctors would have to adjust off patient balances and old insurance claims not including denials for untimely filing issues.
Now let's fast forward to the new era and how to collect your insurance carrier money faster -
1. The charges are entered the same day the patient is treated
2. Charges are scrubbed by medical coding software within minutes notifying the biller of any possible denial issues
3. If patient information is missing or incomplete the claim will not be transmitted to the insurance carrier alerting the biller of these issues
4. All claims get fixed the "same day" and billed to the clearinghouse
5. Clearinghouse scrubs the claims and send any back that do not meet the insurance carriers requirements per their contract with the insurance carrier
6. Within 24 hours those issues are fixed and the denied claims are rebilled
7. The insurance carrier sends a notification of status of claims within 72 hours indicating those that were approved vs. denied
8. Within 5 days of the patients treatment we have notification of the check # the claim will be processed towards
9. Within 10 business days from the date the insurance carrier receives the claim electronically we have an Electronic Remittance Advice along with the date the check will either be mailed to the provider or direct deposited into the providers checking account
10. Patients get a statement normally within 15-20 days of being treated and they pay almost 100% of the time because they actually remember the office visit, they remember what it was for and they realize they have a co-payment, coinsurance or deductible that is owed.
If you are a medical practice and not receiving insurance payments within 25 days of treatment for carriers like Aetna, UHC, Cigna, BCBS, Federal, Medicare, Medicaid, Medi-Cal, Humana or other insurance carriers that accept electronic claims then you need to look for a new billing service, a new Practice Management software or a new clearinghouse based on your results.
Practice Management Software Reviews
Medical Clearinghouse Reviews
1 step to increasing your monthly revenue is to take your billing electronically using a robust clearinghouse that processes eClaims, secondary claims electronically and Electronic Remittance Advice. For more information on how a clearinghouse can help your medical office please check out:
How to read EDI clearinghouse reports
Clearinghouse EDI Reports
Clearinghouse Online Claim Status EDI Reports
Confused by Electronic Medical Claim Billing click here for additional articles on this subject and so much more: electronic medical claim billing
Medical Billing Tags: clearinghouses, practice management software reviews, selecting a practice management software that will make you money, efficient billing strategies, efficient medical billing services, how to be a medical biller, understanding the medical industry and new technologies, medical billing, medical collections, collecting on medical insurance claims, getting faster payments, receiving money faster, sending patient statements quicker, collection letters, reading EDI reports, understanding clearinghouse reports, RelayHealth, McKesson, Faster claims processing, providers, physicians, doctors, medical offices, hospital facilities, claims processing speeds, electronic claims, paper claims, CMS-1500, HCFA 1500, UB-92, UB-04, Institiutional, Professional claims, EDI program edits, minimize the impact, ease of use, reduction of payment errors, data entry errors, pre-edits, scrubbing of claims, claim coding software, medical billing from home, learn how to bill online from anywhere in the world, medical billings and claims, medical billings claims, medical claims electronic billing, claim billing software, electronic medical claim billing, lytec medical billing software, medical billing schools, medical coding and billing schools, medical billing schools online, medical coding and billing schools online, medical billing classes online, online medical billing school, medical billing and coding courses online, courses online, medical billing classes, chiropractic software, online courses medical billing, medical office billing software, medical coding schools, medical coding courses, on line medical billing, medical billing programs, Medicare billing software, medical billing software, medisoft medical billing software, web based medical billing, degree medical billing, electronic medical billing, electronic medical billing software, medical billing education, medical insurance billing software, medical billing and coding course, medical billing online course, medical billing software company, learn medical billing, insurance billing software, medical assistant school, medical billing course, medical billing program, medical billing and coding software, medical billing school, medical billing class, medical billing and coding online, medical billing certificate, medical billing systems, medical billing system, electronic medical claim billing, chiropractic practice management software, medical practice management system, medical practice management software, EMR practice management software, medical practice management services, practice management software, medical billing practice, Aetna Health, health insurance, Auto insurance, Auto Insurance Quotes, Auto insurance quote, Car Insurance Quotes, Commercial Insurance Quote, Car Insurance Quote, Car Insurance Quote, Employers Liability, Employers Liability insurance, Auto Insurance Companies, Property Insurance Quote, Car Insurance Companies, Auto Cheap Insurance, Accident Claim, Liability Insurance Quote, Employer Liability Insurance, Public Liability Insurance, lytec medical, lytec, web based medical billing software, medical billing software, medical billing systems