Florida Medicaid rejection claims missing NPI numbers
As of July 1st 2008 Florida Medicaid has been accepting all electronic claims submitted to them through the Electronic Data Systems (EDS) and your medical office may also receive "997" report notification that claims were accepted. However; what you may not be aware of is that claims missing the provider NPI number are in actuality being rejected or kicked out of their EDS system and are not getting processed for payment.
If you have identified problems with receiving insurance payments on electronic claims from Florida Medicaid after July 1st 2008 please contact the enrollment department to verify your NPI and associated Tax ID numbers are setup correctly in the Florida Medicaid system.
Call Florida Medicaid Provider Enrollment Department at 800-289-7799 option 4 and verify NPI setup. Once everything is setup correctly please rebill all unpaid claims electronically.
Interested in additional Online Medical Billing and Coding articles? Then click out Billing and Coding Online Courses
Medical Billing and Coding Keyword Tags: medical billings and claims, medical billings claims, medical claims electronic billing, claim billing software, electronic medical claim billing, lytec medical billing software, medical billing schools, medical coding and billing schools, medical billing schools online, medical coding and billing schools online, medical billing classes online, online medical billing school, medical billing and coding courses online, courses online, medical billing classes, chiropractic software, online courses medical billing, medical office billing software, medical coding schools, medical coding courses, on line medical billing, medical billing programs, Medicare billing software, medical billing software, medisoft medical billing software, web based medical billing, degree medical billing, electronic medical billing, electronic medical billing software, medical billing education, medical insurance billing software, medical billing and coding course,
Why is it more difficult to get paid than it is to do the work?
ReplyDeleteHi Darrell,
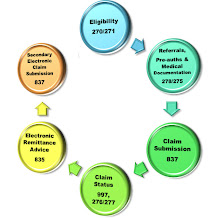
ReplyDeleteInsurance carriers need to find alternative ways of stopping insurance payments to providers. With the streamlined efficiencies of electronic claims, electronic remittance advice (EOB's) and now accepting secondary claims electronically they are paying out more money each month. So, they need to create new loop holes to "stop" paying out.
With this new trend it seems like medical billers and collectors will need to stay involved with EDI agreements, credentialing, contracting rates, allowable fee schedules and so much more! The moment you stop watching is the moment you stop getting paid.
Happy billing/collecting!
Jennifer