Medicare as Secondary Insurance
Has your medical office ever received a request for repayment by the primary insurance carrier; the patient has a secondary insurance through Medicare but was never billed because the primary paid above Medicare's allowed amount so the balance was adjusted off?
Medicare has a 1 year timely filing policy giving most clients ample time to resolve claim issues and submit a clean claim. However; sometimes you will receive a primary insurance payment in full and 2 or 3 years later the insurance carrier will identify they weren't the primary insurance carrier and ask for a full refund. Now what do you do?
For Future Claims take these steps to make sure this never happens to you. Bill Medicare regardless how the primary insurance carrier paid (yes, even if they paid in full.)
- Submit all secondary claims to Medicare even if the primary paid in full
- The medical claim will reflect in Medicare's software to prove timely filing
- Patients might meet part of their deductible even if the primary paid in full and to ease your patients accounting bill the medical claim
- Medicare uses information on the medical claim and submits it to the National Claims Processing File
- If the primary insurance carrier requests a refund at any point you will know you are safe because you have proved timely filing with Medicare
But this has happened to me now - what can I do?
- Take a copy of the Refund Request, EOB's, Claim and any other kind of proof you can show to Medicare that you attempted to collect this correctly through the primary insurance carrier and submit to Medicare.
- If you receive a denial for late filing appeal asking Medicare to waive the claim timely file limit for good cause. Again attach any and all supporting documentation plus a really nice well written appeal letter.
Medicare has the option to evaluate and make a determination based on the supporting documentation.
Medicare states it the doctors responsibility to identify who the correct primary insurance carrier is. Although sometimes the primary insurance carriers are small companies that have slow or bad software programs and they don't update paperwork for weeks or months causing these kinds of issues....
- Always contact the Interactive Voice Response (IVR) and verify files are update
- Contact the Coordination of Benefit Contractor (COBC) (1-800-999-1118) and follow instructions if information is not correct.
- Always bill Medicare as a secondary even if the primary insurance paid in full
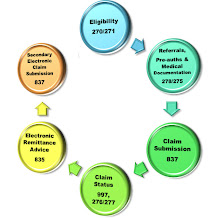
Questions on Electronic Medical Billing and Claims then click here medical claims electronic billing
Key Words: Medicare as secondary insurance carrier, what happens if primary requests a refund and I never billed Medicare, timely filing, late filing, medical claims payment from Medicare, claim submission, bill all claims to Medicare regardless if paid in full, How to appeal Medicare denied claims, Claim Denial, Claim Collection, Coordination of Benefits, COBC, Primary payer, 1 year timely filing, medical claims, medical billing, IVR, proof of timely filing
No comments:
Post a Comment