2430-CAS REQUIRED WHEN 2430-SVD NE 2400-SV102
I am working with a client that received a RelayHealth Payor Message for Montana Medicare as 2430-cas Required when 2430-SVD NE 2400-SV102. She couldn't figure out why she is getting these denials so I reviewed how the patients were setup in the Practice Management software.
- Medicare is the secondary payor for all of these denied claims
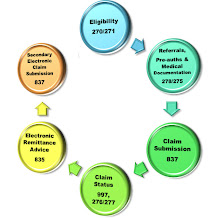
- She has setup to bill Medicare secondary claims electronically
- The Claim Adjustment Reason Codes were not added to the primary payment
Medicare cannot accept these claims electronically because the payment poster did not add the primary payment codes to the claim. Attach the primary claim adjustment reason codes and if you need assistance with what primary claim adjustment reason codes are view my initial blog about this information: Medicare Health Insurance Claim Adjustment Reason Codes
Key Words: Payment Reason Codes, Payment Claim Adjustment Reason Codes, How to fix, Denials, Claim Exclusions, 2430-CAS REQUIRED WHEN 2430-SVD NE 2400-SV102, Medicare claims, secondary payors, electronic claim denials, secondary electronic claims, How to bill, How to receive insurance payments, how to collect on medical claims, how to bill Medical Claims, Learn how to, RelayHealth, Clearinghouse edits, Claim edits, medical claims, practice management secondary claims setup, payer edits, claim payers
Very helpful. Thank You!
ReplyDelete